French scientists have developed a self-setting injectable macroporous foam for repairing bones and aiding its development. It may assist regenerate bone quicker than other materials whereas providing a fast and minimally invasive method for surgeons to carry out bone repair procedures, and possibly treat osteoporosis.
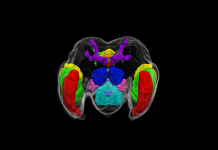
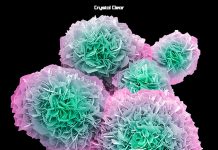
The new study is published in Acta Biomaterialia. Before, scientists had difficulty making calcium phosphate cements (CPCs) macroporous, or having pores larger than 50 micrometers. While studies have found conflicting evidence regarding how porous bones should be to facilitate regrowth, the range seems to be between 100 and 300 micrometers — in people with osteoporosis, bones are far more porous.
With 70% of bone consisting of a calcium phosphate mineral known as hydroxyapatite, CPCs are extensively utilized in surgical procedures as bone substitutes. CPCs have wonderful properties for the job – they’re injectable, self-setting, biocompatible and microporous permitting nutrients to flow through the implant site, which assists bone regeneration.
Nonetheless, it’s been a problem introducing macroporosity into such injectable CPCs, which is desirable to facilitate faster bone regeneration and reinforce cancellous bone; the flexible and spongy tissue that degenerates with osteoporosis. Macroporous CPCs do exist however those which are injectable have poor mechanical properties.
Now Pierre Weiss and colleagues at the University of Nantes have created a macroporous self-setting CPC in the type of an injectable foam by utilizing a silanised-hydroxypropyl methylcellulose (Si-HPMC) hydrogel as a foaming agent. ‘Our method is straightforward and offers us really good outcomes in terms of mechanical properties and macroporous structures,’ says Weiss.
Advantages of bubbles
Previously, the researchers had tried to enhance the mechanical properties of CPC by including a Si-HPMC hydrogel. However in the course of the process of preparing the Si-HPMC hydrogel with an acidic buffer utilizing syringes – which lowers the pH of the solution causing it to self-cross link and gel – air bubbles appeared within the mixture and they had been laborious to remove. However Weiss’ postdocs Jingtao Zhang and Weizhen Liu wondered if this downside may be useful for giving macroporosity to CPC and so they set out to develop a CPC foam.
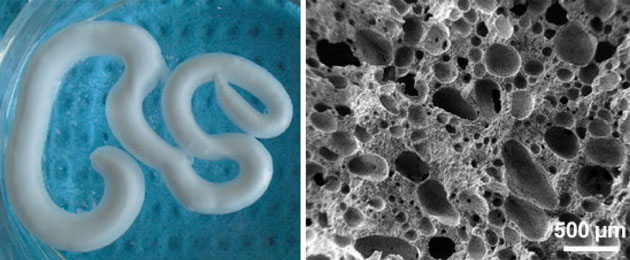
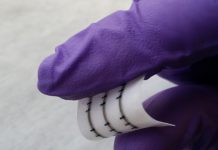
The group made the foam by placing Si-HPMC and CPC solutions in separate syringes, and then pumping air into the CPC syringe. Both syringes were then joined by a connector and plunged to quickly combine the solutions and air, which formed a homogenous foam.
‘We knew that both biomaterials are biocompatible individually however we did not understand how the body would react with a mixture of both,’ explains Weiss. To seek out an answer, and also to check the biofunctionality of the foam, they carried out preliminary in vivo tests by making tiny defects within the thigh bones of two live rabbits and injected the foam into the cavities.
After about a week, the researchers found the foamed CPC had completely filled the defect as well as maintained the macroporous structure they were looking for. After 6 weeks, they found it had acted as a scaffold to facilitate new bone growth; there were newly formed bones within the CPC itself, fitting together uniformly. Analyses revealed no toxic effects, suggesting that the CPC foam might be a feasible and efficient material for treating certain bone defects and ailments. ‘We think this might be an excellent biomaterial, perhaps with active molecules, to act against osteoporosis locally. We have to determine the proof of concept in animal models,’ said Weiss.
‘There are quite a number of teams working on this problem and different solutions proposed. This may very well be one, the preliminary outcomes are very fascinating.’ says Eduardo Saiz, who investigates biomaterials for bone repair at Imperial College, London, UK. ‘If the research progresses well it might give surgeons a simple to use material for minimally invasive procedures, which can benefit clinical practice.’
More research is needed to show just how effective this paste can be, but the team believes it will one day help to prevent some 8 million osteoporosis-related fractures each year across the globe.
Source: J Zhang et al, Acta Biomater., 2015, DOI: 10.1016/j.actbio.2015.11.055




































Thank Mr Skeltal